Crohn’s Disease and Ulcerative Colitis Diagnosis
| ✅ Paper Type: Free Essay | ✅ Subject: Medical |
| ✅ Wordcount: 3750 words | ✅ Published: 23 Sep 2019 |
Critically appraise the diagnosis of Crohn’s Disease and Ulcerative Colitis
Assess the value or quality of….
Inflammatory bowel disease (IBD) affect more than 300,000 people in the UK (Fakhoury et al, 2014.) IBD is known as a chronic intestinal inflammation that is a result of host-microbial interactions (Fakhoury et al, 2014.) These diseases are autoimmune and cause inflammation in the small and large intestines.
Two main forms of inflammatory bowel disease are Crohn’s Disease (CD) and Ulcerative Colitis (UC). They cause symptoms such as abdominal pain, bloody stools, diarrhea and vomiting (Fakhoury et al, 2014.) Both conditions share similar characteristics however differentiation can be made when it comes to the location and the type of inflammation. Crohn’s Disease causes inflammation anywhere along the lining of the digestive tract whereas ulcerative colitis causes a long-lasting inflammation in some parts of the tract, mainly the colon (Garud and Pppercorn, 2009.) These diseases normally occur during adulthood however there has been an increase in the diagnosis of children. As both conditions share symptoms diagnosis can be difficult so a proper examination has to be conducted to ensure the correct disease is identified helping to provide effective treatment. To do this, special diagnostic techniques need to be conducted, some techniques that are used are discussed in further depth below accompanied by brief methods, results gained and their efficacy in the role of diagnosis for both CD and UC.
Table 1- The difference in the findings of patients with CD and UC (Adapted from Zhang et al, 2018.)
A simple presentation of the differences found between both conditions upon examination.
|
Key features |
Crohns’ disease |
Ulcerative colitis |
|
Histologic findings |
Presence of Granulomas Transmural inflammation |
Mucosal and submucosal inflammation Polymorphonuclear cell aggregate |
|
Endoscopic findings |
Strictures Liner ulcerations Discontinues lesions |
Presence of crypts Formation of residual mucosal tissue Continuous lesions |
There are many techniques and tests which can be used to identify IBD however the family history of the patient can be looked at. Some studies have shown that UC patients hafve a family history of IBD in comparison to patients with Crohns disease (Childers et al, 2014.) This could be a good start to help diagnose the patient as a little background information is provided.
Crohn’s Disease can be effectively diagnosed using a capsule endoscopy however the clinical use of this technique in patients with ulcerative colitis is unclear. Research conducted on patients with UC showed small bowel finding which are normally consistent in Crohn’s Disease (Mehdizadeh et al, 2008) which suggest this method should be used less, if UC is suspected or along with this test further examination should be done for confirmation. The patient is made to drink a formulation so that the colon is clean prior the endoscopy. The capsule is orally ingested and takes images of the inner layer of the gastrointestinal tract (Fakhoury et al, 2014.) The images captured help to highlight any ulcerations as shown in figure 1, erosions, cankers, fistulas or pseudopolyps which can help identify the location of the inflammation (Fakhoury et al, 2014.)

Figure 1- Crohn’s Disease patients suffering from lesions. (Lujan- sanchis et al, 2016.)
Capsule endoscopy was done capturing 3 different types of lesions. Image A shows the presence of Edema. This is the inflammation of the tract lining which is due to the small blood vessels leaking fluid into the nearby tissues of the digestive tract. Image B shows the ulcers created in the lining. The immune system of the patient attacks the lining causing the formation of ulcers. Ulcers can go onto create fistulas if they manage to break through the intestinal wall. The presence of a fistula can cause food to bypass areas of the bowel which results in inefficient absorption of the nutrients (Soloman, 1996.) Lastly, image C shows strictures. This is the buildup of scar tissue in the wall of the small or large intestines. Long term inflammation causes damage which the body tries to repair but only leads to the buildup of the damaged tissue (Chang et al, 2015.) This lesion can cause a narrowing anywhere in the digestive tracts which will need opening by surgery.
Blood tests are good laboratory tests used to help with the identification of both UC and CD. Any abnormal levels of a particular component can help to identify the presence of a problem. Erythrocyte sedimentation rates (ESR) is an indicator of inflammation. ESR helps to reflect the change of various acute phase proteins. The usefulness of this test has decreased however it is still widely used (Cioffi, 2015.)
The full blood count of the patient can be reviewed and if signs of anemia caused by vitamin B12 deficiency is revealed then further investigation can be conducted to specifically identify the reason behind the anemia (Fakhoury et al, 2014.). Furthermore, any abnormal levels of serological markers can be used to differentiate between both conditions making it easier to diagnose (Fakhoury et al, 2014) which are spoken about below in more detail.
Antibody tests can be done to help differentiate between both diseases. Anti-Saccharomyces cerevisiae antibodies (ASCA) is a protein that is present in people who have Crohn’s Disease whereas Perinuclear anti-neutrophil cytoplasmic antibody (pANCA) is the protein which is present when individuals have ulcerative colitis (Quinton et al, 1998.). The presence of ASCA is not clear so a family study was conducted which showed that the presence of ASCA may be due to genetic influence along with the influence of environmental factors (Seibold, 2001.) The presence of pANCA is still controversial however research has shown that this protein is sensitive and specific to the diagnosis of UC (Yamamoto-Furusho, 2006.)
Presence of these proteins can help to push the doctors in the correct direction when it comes to the patient’s diagnosis.
Elevated white blood cell level and C-reactive protein along with a decrease in albumin help to suggest a diagnosis. Other specific serum markers for each disease can be looked into for the presence of inflammation and acute phase response (Cioffi, 2015.) For UC the stool of the patient can be cultured to rule out the presence of any infection (Collins, Paul and Rhodes, 2006.)
Another diagnostic tool is radiology tests. Fluoroscopic examinations are infrequently performed but can help to suggest the possible cause of the problem. A barium enema is conducted. For this test the patient is either required to consume a solution of barium sulfate and then an x-ray is conducted, or an enema tube is inserted into the rectum which flows through the colon and takes x-rays (Eliakim et al, 2003.) The barium appears white when an X-ray is conducted helping to easily view the problematic areas to see any ulcers, narrowed areas or any fistulas (Eliakim et al, 2003) which are visible in figure 2. Further examination of the X-rays can be done to help identify the spread of the disease however this technique is not used often as the positive oral contrasting agent can obstruct the presentation of mucosal enhancement or any hemorrhage (IIangovan, 2012.)
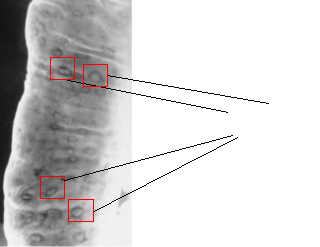
Figure 2- the presence of Aphthous ulcers.
Barium Enema examination was conducted on a patient with Crohn’s Disease which showed the presence of many ulcers. (https://emedicine.medscape.com/article/367666-overview)
As technology has advanced radiology techniques such as X-ray computed tomography (CT) and magnetic imaging scans (MRI) are used to look for abnormalities caused by the IBD’s.
The preferred imaging tests to help with the diagnosis are cross-sectional CT and MR Enterography. CT enterography is preferred when an adult is examined because it is less dependent on bowel and respiratory motion and it is noninvasive however high-quality MR Enterography eliminates radiation exposure and is as sensitive as CT enterography which suggests it’s a better method to use (IIangovan et al, 2012.) Both techniques are performed after an oral contrast liquid is consumed by the patient so a high-resolution image is produced (IIangovan et al, 2012.)
CTs utilize multi detector scanners with high spatial and temporal resolution to allow the visualization of the mucosa, small bowel wall and lumen to help detect the severity of the inflammation, fibrofatty proliferation, sacculations and submucosal fat deposition which is a good indicator of chronic inflammation (Ilangovan, 2012.) This technique is known to provide complementary diagnosis after the use of MRI and capsule endoscopy. Low-density oral contrast media helps to create a good quality scan as they maximize contrast between the lumen and enhancing small bowel wall along with helping with the assessment of the wall thickening or any enhancement (Ilangovan, 2012.)
Magnetic resonance imaging (MRI) is a technique which helps to produce high quality images identifying any abscess or fistulas without exposing the patient to radiation (Eliakim et al, 2003.) It has spatial and temporal resolution of images which can help to evaluate the bowel wall changes, thickening and any edema which can be useful to assess the IBD activity.
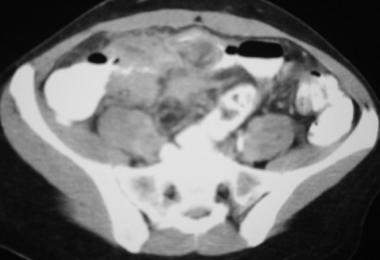
Figure 3- CT scan conducted on a patient with Crohn disease. https://emedicine.medscape.com/article/367666-overview#a1
This scan shows mesenteric inflammation in the lower right of the ileum along with thickening of the wall and narrowing of the terminal ileum.
Another technique used to diagnosis is transabdominal ultrasound. This can help to detect complications being caused by the inflammatory bowel diseases and it is said that the ultrasound can help to distinguish between UC and CD purely based on the thickness and the change of layered structure of the intestines (Kimmey et al, 1990.) The ultrasound appears to be accurate in being able to differentiate between a normal and inflamed colon however this technique cannot be used solely to diagnose an individual so further tests should be conducted. Ultrasounds are good at detecting the build up of fluids along with helping to show up fistulas and abscessed which maybe present.
Enteroscopy is a major tool which is used to detect and manage IBD. It plays a crucial part in the diagnosis as it can help to distinguish between CD and UC along with helping with long term management. The procedure for this method is the insertion of a tube containing a camera through the mouth to observe the GI tract, this is defined as upper enteroscopy. Lower enteroscopy is used to view the colon and the camera is inserted through the anus. This procedure is relatively pain free however cause discomfort.
Colonoscopy is the first line endoscopic investigation when CD is suspected whereas for UC flexible sigmoidoscopy is used then accompanied by colonoscopy. Colonoscopy plays many roles when used to investigate IBD such as: assessment of the extent and activity of the disease, surveillance of dysplasia or neoplasia, diagnosis and then to help with the correct treatment (Rameshshanker and Arebi, 2012.)
Endoscopic findings of active UC consist of loss of the vascular pattern due to oedema, ulceration, bleeding and erythema (Rameshshanker and Arebi, 2012.) The findings can help to show the distribution of inflammation which furthermore help to conclude if it’s CD or UC. Chronic UC can be diagnosed with the presence of polyps, scarring and shortening of the tubular colon as shown in figure 4.
Whereas on the other hand, CD can cause inflammation anywhere along the GI tracts so when an endoscopy is conducted the inflammation pattern is observed. Other identification pointers are the presence of heterogeneous patchy nature of inflammation or skip lesions, along with presentation of polycyclic ulcers (Rameshshanker and Arebi, 2012.) The ulcers are deeps as shown in figure 5 when compared to the UC ulcers in figure 4.
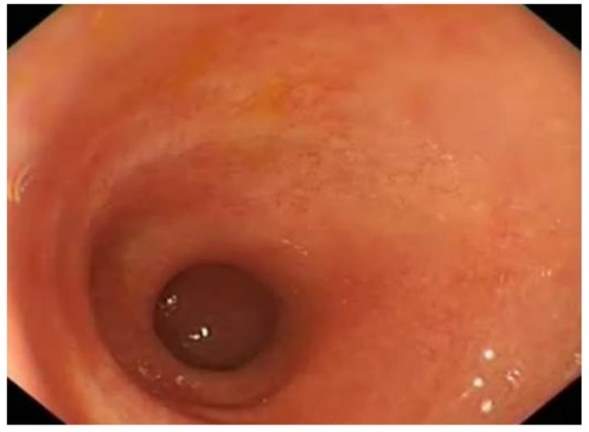
Figure 4- The endoscopic finding consisting of a shortened tubular colon in a patient with UC.
It is clearly visible that as the patient is suffering from the disease as a huge amount of inflammation has taken place which reduces the surface area of the colon, making it difficult for the colon to function. This will reduce the amount of fluid reasorption and there will be an incomplete production of waste that the body needs to eliminate causing further build up of waste. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3377861/
Patients suffering with UC have the possibility to develop colorectal cancer. By conducting an endoscopy to provide the correct diagnosis, the treatment needed can be provided, monitoring the progression of the patients condition and determining colonoscopy markers for cancer risk can decrease the risk of the patient (Rutter et al, 2004.)

Figure 5- Deeps ulcers are observed along with sub mucosal oedema and haemorrhages in the colon of a patient with Crohn’s Disease. CD has caused an immune response in the individual resulting in the production of ulcers along with swelling. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3377861/
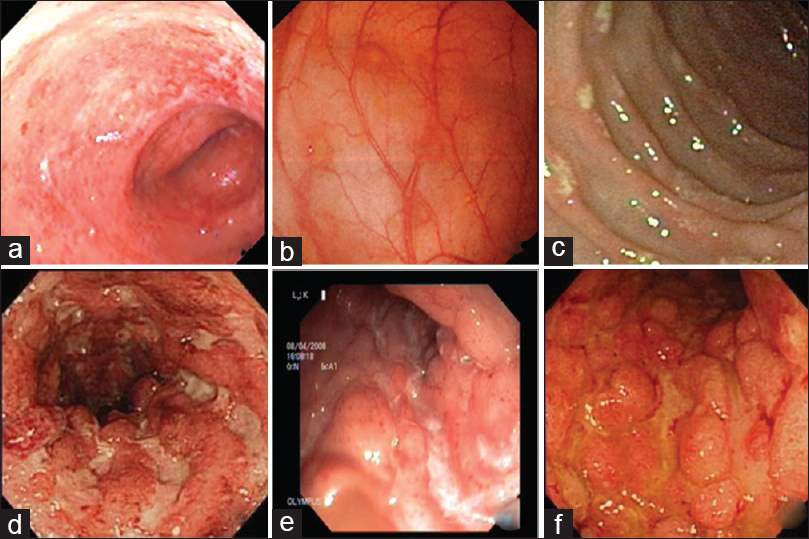
Figure 6- The endoscopic findings of a patient which was diagnosed with Crohn’s disease.
Image A shows erythema along with the loss of vascular with image B demonstrating the presence of aphthous ulcers in the colon and C showing the presence of discrete ulcers (Moka, Ahuja and Makharia, 2017.) Image D and E show the presence of multiple deep ulcers and finally F shows a cobblestone apprearnce of the colon (Moka, Ahuja and Makharia, 2017.) http://www.jdeonline.in/article.asp?issn=0976-5042;year=2017;volume=8;issue=1;spage=1;epage=11;aulast=Moka
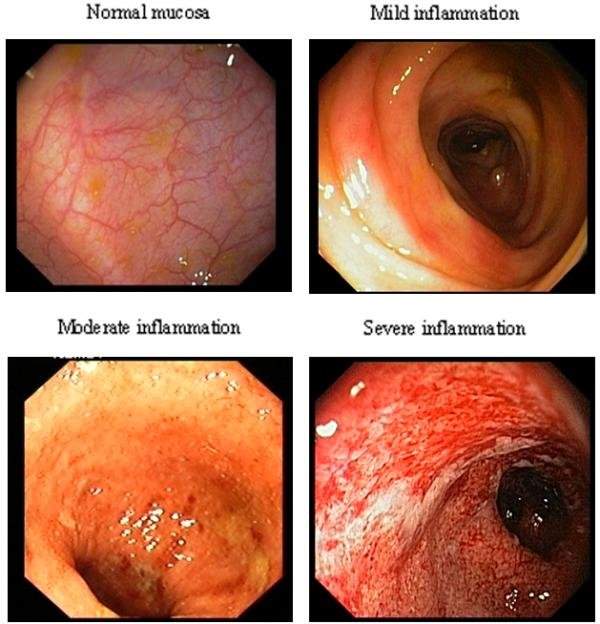
Figure 7- The images captured after endoscopy is performed on patients with ulcerative colitis (Lange, Larsen and Aabakken, 2004.)
5 patients who were suffering from ulcerative colitis at different degrees underwent an endoscopic examination. The amount of inflammation that was ongoing in the patient was recorded as shown above, to present the different stages of ulcerative colitis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC434504/

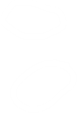
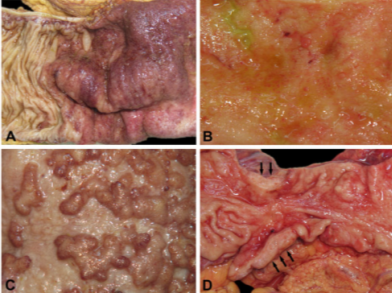
Figure 8- The examination of a specimen in UC which is a presentation of chronic inflammation along with the production of abnormal mucosa.
A shows the granular appearance of the mucosa along with ulceration occurring in the tissue, B shows extensive ulceration and the rise of inflammatory polyps. C shows the long-lasting effect of the disease as the mucosa is lacking haustration and it is atrophic lastly, D shows the start of adenocarcinoma highlighted in the figure. (Langner et al, 2014.) https://www.ncbi.nlm.nih.gov/pubmed/24487791
Endoscopic findings as spoken about above are important to help evaluate the activity of both diseases. Figure 6 and 7 especially highlight the value of endoscopy to help diagnose a patient as they clearly demonstrate the difference in the findings of both conditions. The images captured during the examination can help to ease doctors in the diagnosis of a patient. There is potential for the condition of the patient to overlap and make it harder for diagnosis hence why other tests should be considered.
A histology approach can be taken towards inflammatory bowel diseases. Biopsies of the colon can be conducted during an endoscopy test to take a look at the change in the structure of the tissue. An effective technique used to both, differentiate between the types of inflammation and diagnose the disease (Fakhoury et al, 2014.) Specific aspects of the pathology can help to identify the inflammation that occurs when an individual has CD or UC. Multiple samples can be taken along the lining to examine inflammation which can suggest CD and then samples of the colon can be taken which can suggest UC. The samples can be stained then viewed under a microscope as shown in figure 9. The biopsy samples should be taken before the start of any treatment as this can induce a morphological change in the structure of the tissue.

Figure 9- the identification of Granulomas in Crohn’s Disease when a sample from the stomach is taken and stained.
After the biopsy sample was stained using the Hematoxylin and eosin stain, further analysis helps to highlight mucosal damage which is due to the infiltration of leukocytes into the epithelium along with the presence of macrophage Granulomas (Fakhoury et al, 2014.) As mentioned in Table 1, one of the biggest identification pointers of CD being present is the presence of granulomas which has been identified in this patient’s case providing the correct diagnosis.
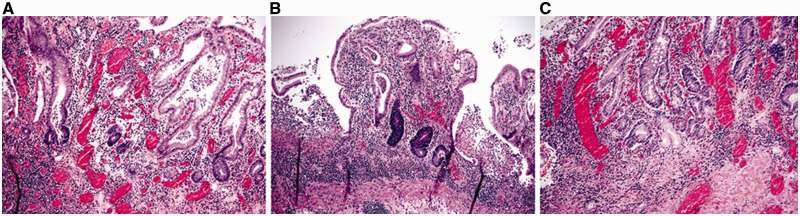
Figure 10- The images captured after the examination of tissue from a patient suffering from ulcerative colitis. Image A and B show architectural distortion, variation when it comes to the size of the crypts and basal lymphoplasmacytosis along with C showing metaplasia in the Paneth cell and pyloric gland in the left colon (Deroche, Xiao and Liu, 2014.) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4124271/
The differences captured after the microscopy of the patient’s sample is done helps to show some key markers such as granulomas as shown in figure 9 or the distortion shown in figure 10 can help to clarify any confusion there may be in the diagnosis of the condition.







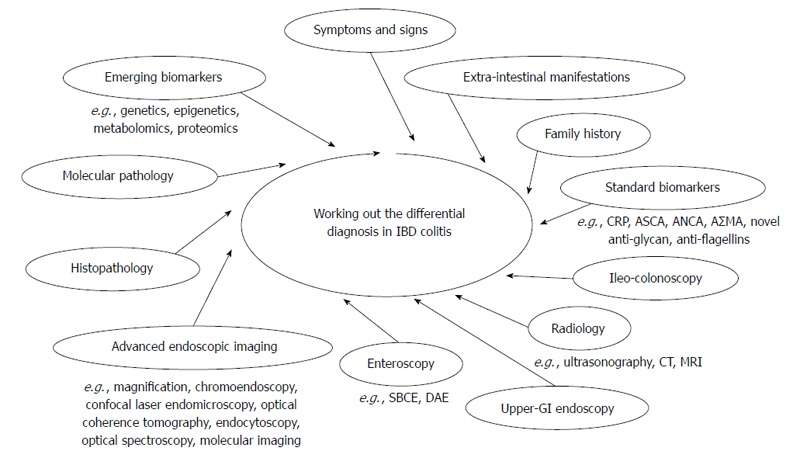
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284336/
References
- Chang, C.W., Wong, J.M., Tung, C.C., Shih, I.L., Wang, H.Y. and Wei, S.C., 2015. Intestinal stricture in Crohn’s disease. Intestinal research, 13(1), pp.19-26, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4316217/ [Accessed 7/01/2019]
- Cioffi, M., De Rosa, A., Serao, R., Picone, I. and Vietri, M.T., 2015. Laboratory markers in ulcerative colitis: Current insights and future advances. World journal of gastrointestinal pathophysiology, 6(1), p.13, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4325297/ [Accessed at 21/12/2018]
- Collins, P. and Rhodes, J., 2006. Ulcerative colitis: diagnosis and management. BMJ: British Medical Journal, 333(7563), p.340, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1539087/ [Accessed 29/12/2018]
- De Lange, T., Larsen, S. and Aabakken, L., 2004. Inter-observer agreement in the assessment of endoscopic findings in ulcerative colitis. BMC gastroenterology, 4(1), p.9, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC434504/ [Accessed 25/12/2018]
- DeRoche, T.C., Xiao, S.Y. and Liu, X., 2014. Histological evaluation in ulcerative colitis. Gastroenterology report, 2(3), pp.178-192, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4124271/ [Accessed 26/12/2018]
- Eliakim, R., Fischer, D., Suissa, A., Yassin, K., Katz, D., Guttman, N. and Migdal, M., 2003. Wireless capsule video endoscopy is a superior diagnostic tool in comparison to barium follow-through and computerized tomography in patients with suspected Crohn’s disease. European journal of gastroenterology & hepatology, 15(4), pp.363-367, [Online] Available at https://www.webmd.com/ibd-crohns-disease/crohns-disease/crohns-disease-diagnosis#2 [Accessed 27/12/2018]
- Fakhoury, M., Negrulj, R., Mooranian, A. and Al-Salami, H., 2014. Inflammatory bowel disease: clinical aspects and treatments. Journal of inflammation research, 7, p.113, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4106026/ [Accessed 1/01/2019]
- Garud, S. and Peppercorn, M.A., 2009. Ulcerative colitis: current treatment strategies and future prospects. Therapeutic advances in gastroenterology, 2(2), pp.99-108, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3002512/ [Accessed 26/12/2018]
- Ilangovan, R., Burling, D., George, A., Gupta, A., Marshall, M. and Taylor, S.A., 2012. CT enterography: review of technique and practical tips. The British journal of radiology, 85(1015), pp.876-886, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3474054/ [Accessed 9/01/2019]
- Kimmey, M.B., Wang, K.Y., Haggitt, R.C., Mack, L.A. and Silverstein, F.E., 1990. Diagnosis of inflammatory bowel disease with ultrasound. An in vitro study. Investigative radiology, 25(10), pp.1085-1090, [Online] Available at https://www.ncbi.nlm.nih.gov/pubmed/2079406 [Accessed 28/12/2018]
- Luján-Sanchis, M., Sanchis-Artero, L., Larrey-Ruiz, L., Peño-Muñoz, L., Núñez-Martínez, P., Castillo-López, G., González-González, L., Clemente, C.B., Antequera, C.A., Durá-Ayet, A. and Sempere-Garcia-Argüelles, J., 2016. Current role of capsule endoscopy in Crohn’s disease. World journal of gastrointestinal endoscopy, 8(17), p.572, [Online] Available at https://www.wjgnet.com/1948-5190/full/v8/i17/572.htm [Accessed 5/01/2019]
- Mehdizadeh, S., Chen, G., Enayati, P.J., Cheng, D.W., Han, N.J., Shaye, O.A., Ippoliti, A., Vasiliauskas, E.A., Lo, S.K. and Papadakis, K.A., 2008. Diagnostic yield of capsule endoscopy in ulcerative colitis and inflammatory bowel disease of unclassified type (IBDU). Endoscopy, 40(01), pp.30-35, [Online] Available at https://www.ncbi.nlm.nih.gov/pubmed/18058654 [Accessed 4/01/2019]
- Moka, P., Ahuja, V. and Makharia, G.K., 2017. Endoscopic features of gastrointestinal tuberculosis and crohn’s disease. Journal of Digestive Endoscopy, 8(1), p.1, [Online] Available at http://www.jdeonline.in/article.asp?issn=0976-5042;year=2017;volume=8;issue=1;spage=1;epage=11;aulast=Moka [Accessed 2/01/2019]
- Quinton, J.F., Sendid, B., Reumaux, D., Duthilleul, P., Cortot, A., Grandbastien, B., Charrier, G., Targan, S.R., Colombel, J.F. and Poulain, D., 1998. Anti-Saccharomyces cerevisiae mannan antibodies combined with antineutrophil cytoplasmic autoantibodies in inflammatory bowel disease: prevalence and diagnostic role. Gut, 42(6), pp.788-791, [Online] Available athttps://www.webmd.com/ibd-crohns-disease/crohns-disease/crohns-disease-diagnosis#1 [Accessed 25/12/2018]
- Rameshshanker, R. and Arebi, N., 2012. Endoscopy in inflammatory bowel disease when and why. World journal of gastrointestinal endoscopy, 4(6), p.201, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3377861/ [Accessed 9/01/2019]
- Rutter, M.D., Saunders, B.P., Wilkinson, K.H., Rumbles, S., Schofield, G., Kamm, M.A., Williams, C.B., Price, A.B., Talbot, I.C. and Forbes, A., 2004. Cancer surveillance in longstanding ulcerative colitis: endoscopic appearances help predict cancer risk. Gut, 53(12), pp.1813-1816, [Online] Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1774334/ [Accessed 2/01/2019]
- Solomon, M.J., 1996. Fistulae and abscesses in symptomatic perianal Crohn’s disease. International journal of colorectal disease, 11(5), pp.222-226, [Online] Available at https://www.ncbi.nlm.nih.gov/pubmed/8951512 [Accessed 6/01/2019]
- Zhang, J., Huang, J., Aximujiang, K., Xu, C., Ahemaiti, A., Wu, G., Zhong, L. and Yunusi, K., 2018. Thyroid Dysfunction, Neurological Disorder and Immunosuppression as the Consequences of Long-term Combined Stress. Scientific reports, 8(1), p.4552, [Online] Available at https://www.nature.com/articles/s41598-018-19564-y [Accessed 31/12/2018]
- https://academic.oup.com/ecco-jcc/article/8/11/1480/357277 Childers, R.E., Eluri, S., Vazquez, C., Weise, R.M., Bayless, T.M. and Hutfless, S., 2014. Family history of inflammatory bowel disease among patients with ulcerative colitis: a systematic review and meta-analysis. Journal of Crohn’s and Colitis, 8(11), pp.1480-1497.
- https://www.ncbi.nlm.nih.gov/pubmed/11252413 Seibold, F., Stich, O., Hufnagl, R., Kamil, S. and Scheurlen, M., 2001. Anti-Saccharomyces cerevisiae antibodies in inflammatory bowel disease: a family study. Scandinavian journal of gastroenterology, 36(2), pp.196-201.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4087873/ Yamamoto-Furusho, J.K., Takahashi-Monroy, T., Vergara-Fernandez, O., Reyes, E. and Uscanga, L., 2006. Perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA) in chronic ulcerative colitis: experience in a Mexican institution. World Journal of Gastroenterology: WJG, 12(21), p.3406.
- https://www.ncbi.nlm.nih.gov/pubmed/24487791 Langner, C., Magro, F., Driessen, A., Ensari, A., Mantzaris, G.J., Villanacci, V., Becheanu, G., Nunes, P.B., Cathomas, G., Fries, W. and Jouret-Mourin, A., 2014. The histopathological approach to inflammatory bowel disease: a practice guide. Virchows Archiv, 464(5), pp.511-527. histimage
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal


